MBARARA CITY, March 31, 2025 – – Mbarara Regional Referral Hospital [ MRRH ], found in Mbarara City, has received a newly constructed extension of children’s paediatric ward from Bethany Kids Uganda, a Christian mission transforming the lives of African children with surgical conditions and disabilities through pediatric surgery.
According to Ivan Nuwagaba, the Country Director Bethany Kids, the new annex paediatric ward worth Shs 60 million is a commemoration of Martin S. Situma, founder of Mbarara paediatric surgical unit at MRRH who passed on July 21, 2022.
“We stand to remember the great work and the impact done by Dr Martin Situma who started this in 2014. We want to commemorate the great work and the impact the Bethany Kids has had since 2014,” Nuwagaba noted.
He said, “Their core area is paediatric surgery, rehabilitation and spiritual support. This facility is one of the milestones recorded under rehab and surgery. We shall continue with the work that he did and the impact that is it is having in the community.”
Nuwagaba said that the children’ paediatric surgery unit was congested and called for an extension of the unit to accommodate more malformed children.
“Over time, our care has been growing and the numbers of malformed children coming here for care have been increasing but we didn’t have enough space. So, Bethany Kids came in to provide an extension to have enough space to accommodate a good number of these children,” he emphasised.
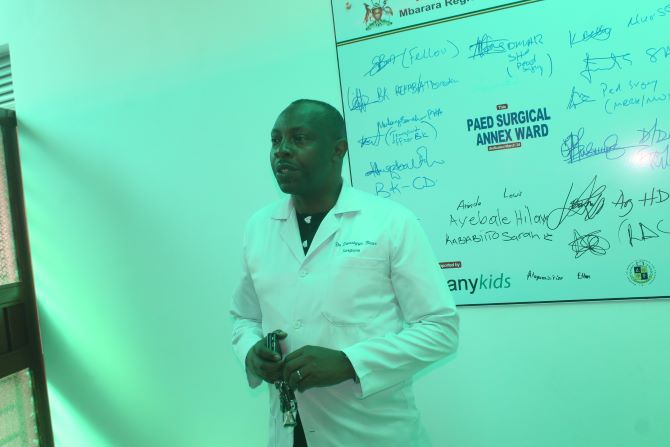
Dr Felix Oyania, Paediatric Surgeon at Mbarara University of Science and Technology [MUST] and MRRH thanked Bethany Kids’ support, saying it will enhance quality healthcare at the hospital.
He said that they had a 14-bed capacity operating only 70-100 cases of malformations per month. “Thank you so much Bethany Kids Uganda, we convey our sincere appreciation to Mbarara University because we are beneficiaries of the cordial relationship. We hope that through this extension, we are going to increase the number of surgeries to 150 per month,” Oyania noted.
“This extension is going to improve the care for our patients in south western region and beyond, of course, free of charge,” he added
According to medics, malformations in children is a condition where babies are born with congenital anomalies [things that go wrong] when they are still in their mothers’ womb. Among these include: anorectic malformation, gastroschisis, oesophageal atresia, and omphalocele among others.
“There are so many malformations of course there are those which are acquired as they grow,” Oyania said.
Causes of malformations
According to Dr Oyania, there is no specific cause of malformations among children. “Others may be environmental, some are genetic, some come as a result of the foods that we eat, the chemicals that are around, alcohol, toxins like smoking among others. So, the anomalies are many but we take care of them here at the unit,” he noted.
On his part, Dr Jonan Tusiimire, Deputy Dean Faculty of Medicine at MUST, rallied the people out there to always bring their children with malformations at MRRH for the specialised care free of charge.
“I would like to communicate to the entire public that we are offering services for children who have different malformations that need surgery. So please bring those children here because the services are available. We hope that collectively, we are going to improve the health of children in our communities,” Tusiimire explained.
Dr Deus Twesigye – Acting Executive Director, MRRH, commended the tripartite partnership between MUST, MRRH, and Bethany Kids Uganda for establishing a modern facility for malformation surgeries.
Additional info:
Key facts
- An estimated 240 000 newborns die worldwide within 28 days of birth every year due to congenital disorders. Congenital disorders cause a further 170 000 deaths of children between the ages of 1 month and 5 years.
- Congenital disorders can contribute to long-term disability, which takes a significant toll on individuals, families, health care systems and societies.
- Nine of ten children born with a serious congenital disorder are in low- and middle-income countries.
- As neonatal and under-5 mortality rates decline, congenital disorders become a larger proportion of the cause of neonatal and under-5 deaths.
- The most common severe congenital disorders are heart defects, neural tube defects and Down syndrome.
- Although congenital disorders may be the result of one or more genetic, infectious, nutritional or environmental factors, it is often difficult to identify the exact causes.
- Some congenital disorders can be prevented. Vaccination, adequate intake of folic acid or iodine through fortification of staple foods or supplementation, and adequate care before and during a pregnancy are examples of prevention methods.
Prevention
Preventive public health measures work to decrease the frequency of certain congenital disorders through the removal of risk factors or the reinforcement of protective factors. Important interventions and efforts include:
- ensuring adolescent girls and mothers have a healthy diet including a wide variety of vegetables and fruit, and maintain a healthy weight;
- ensuring an adequate dietary intake of vitamins and minerals, particularly folic acid in adolescent girls and mothers;
- ensuring mothers avoid harmful substances, particularly alcohol and tobacco;
- avoidance of travel by pregnant women (and sometimes women of child-bearing age) to regions experiencing outbreaks of infections known to be associated with congenital disorders;
- reducing or eliminating environmental exposure to hazardous substances (such as heavy metals or pesticides) during pregnancy;
- controlling diabetes prior to and during pregnancy through counselling, weight management, diet and administration of insulin when required;
- ensuring that any exposure of pregnant women to medications or medical radiation [such as imaging rays] is justified and based on careful health risk–benefit analysis;
- vaccination, especially against the rubella virus, for children and women;
- increasing and strengthening education of health staff and others involved in promoting prevention of congenital disorders; and
- screening for infections, especially rubella, varicella and syphilis, and consideration of treatment.
Screening, treatment and care
Screening
Health care before and near conception (preconception and peri-conception) includes basic reproductive health practices, as well as medical genetic screening and counselling. Screening can be conducted during the 3 periods listed:
- Preconception screening:
This can be useful to identify those at risk of specific disorders or of passing a disorder onto their children. Screening includes obtaining family histories and carrier screening and is particularly valuable in countries where consanguineous marriage is common.
- Peri-conception screening:
Maternal characteristics may increase risk, and screening results should be used to offer appropriate care, according to risk. This may include screening for young or advanced maternal age, as well as screening for use of alcohol, tobacco or other risks. Ultrasound can be used to screen for Down syndrome and major structural abnormalities during the first trimester, and for severe fetal anomalies during the second trimester. Maternal blood can be screened for placental markers to aid in prediction of risk of chromosomal abnormalities or neural tube defects, or for free fetal DNA to screen for many chromosomal abnormalities. Diagnostic tests such as chorionic villus sampling and amniocentesis can be used to diagnose chromosomal abnormalities and infections in women at high risk.
- Neonatal screening:
Screening of newborns is an important step towards detection. This helps to reduce mortality and morbidity from congenital disorders by facilitating earlier referral and the initiation of medial or surgical treatment.
Early screening for hearing loss provides an opportunity for early correction and allows the possibility of acquiring better language, speech and communication skills. Early screening of newborns for congenital cataract also allows early referral and surgical correction which increases the likelihood of sight.
Newborns may be screened for certain metabolic, hematologic and endocrine disorders, many of which may not have immediately visible effects. The conditions screened for vary by country, depending on prevalence and cost. Newborn screening is increasingly conducted even in low- and middle-income countries.
Treatment and care
Some congenital disorders can be treated with medical or surgical interventions. Access to this care may vary by country and by different levels of a health system, though complex care is increasingly available in low- and middle-income settings.
Surgery with good follow up care can often mitigate the potential lethality [as in the case of congenital heart defects] or the morbidity [e.g., congenital talipes, cleft lip/palate] associated with structural congenital disorders. The contribution to reducing mortality and morbidity of this aspect of the treatment is often underestimated. Outcomes are improved with early detection at lower levels of the system through screening, referral and management [at specialist centres in case of some issues like cardiac defects].
Medical treatment for certain metabolic, endocrine and hematological conditions can improve quality of life. A clear example is congenital hypothyroidism, where early detection and treatment allows full physical and mental development to healthy adulthood, whereas a missed diagnosis or unavailability of a simple treatment carries a risk of serious intellectual disability.
Children with some types of congenital disorders may require long term support including physical therapy, speech therapy, occupational therapy and support from families and community.
WHO response
Through the resolution on birth defects of the Sixty-third World Health Assembly [2010], Member States agreed to promote primary prevention and improve the health of children with congenital disorders by:
- developing and strengthening registration and surveillance systems;
- developing expertise and building capacity for the prevention of congenital disorders and care of children affected;
- raising awareness on the importance of newborn screening programmes and their role in identifying infants born with congenital disorders;
- supporting families who have children with congenital disorders and associated disabilities; and
- strengthening research on major birth defects and promoting international cooperation in combatting them.
Together with partners, WHO convenes annual training programmes on the surveillance and prevention of congenital disorders. WHO is also working with partners to provide the required technical expertise for the surveillance of neural tube defects, for monitoring fortification of staple foods with folic acid, and for improving laboratory capacity for assessing risks for folic acid-preventable congenital disorders and is assisting low- and middle-income countries in improving control and elimination of rubella and congenital rubella syndrome through immunisation.
https://thecooperator.news/no-ebola-cases-at-mbarara-hospital-director-confirms/
Buy your copy of thecooperator magazine from one of our country-wide vending points or an e-copy on emag.thecooperator.news